- +91-11-4044-5999
- info@cdri.world
-
Copernicus Marg, New Delhi, INDIA
Strategic Initiatives



The Global Infrastructure Resilience Report addresses a crucial void in the ongoing discourse on infrastructure resilience by providing a compelling argument from economic, financial, and political perspectives for prioritizing investments in resilience. It brings together an unprecedented collection of evidence, delivering a strong case to significantly increase infrastructure resilience investments.

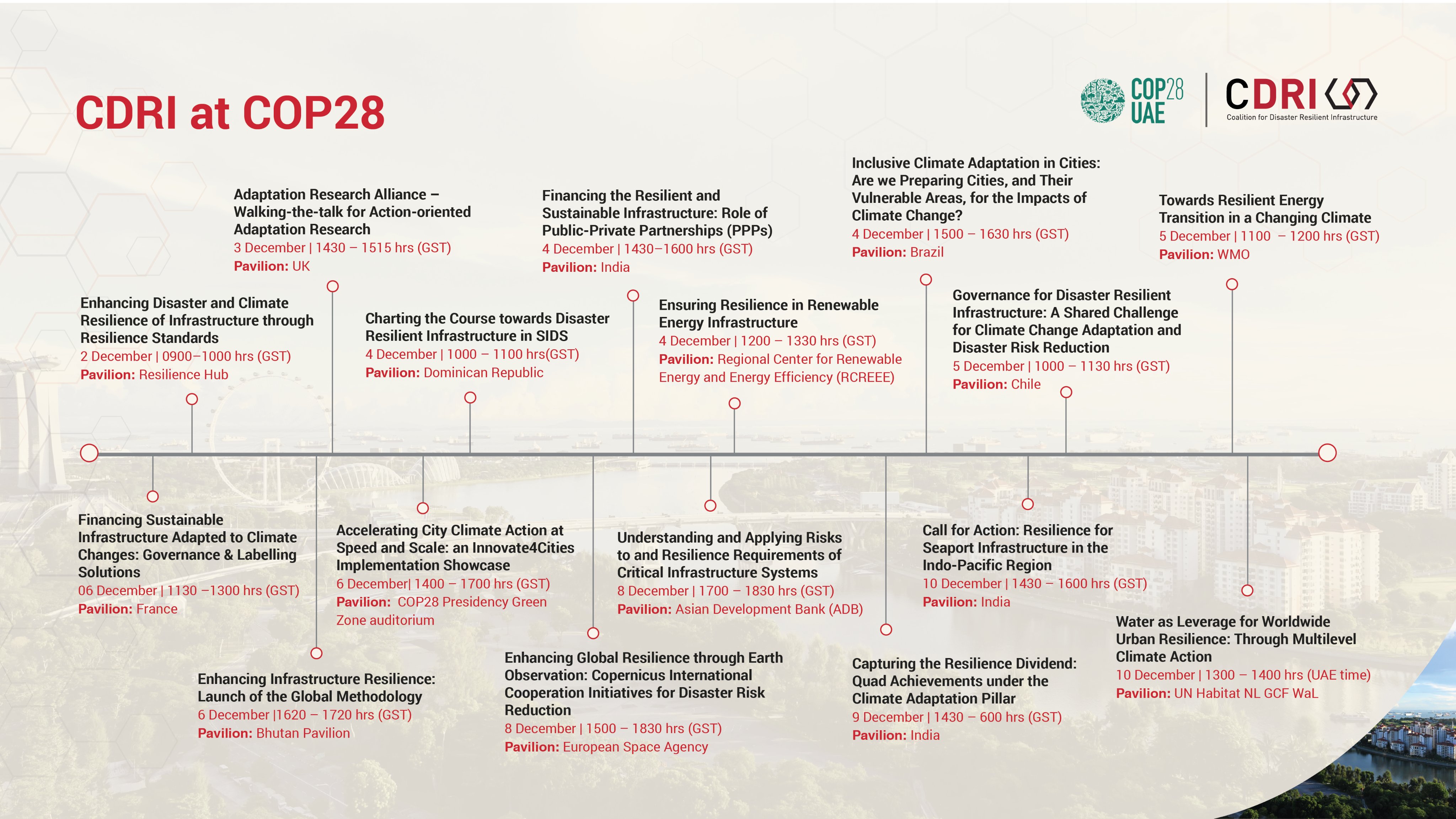
IRIS was jointly launched at the World Leaders Summit at COP26 in Glasgow, UK, by the Prime Ministers of India, UK, Australia, Fiji, Jamaica and Mauritius. IRIS is a dedicated initiative that aims to support Small Island Developing States (SIDS) in achieving sustainable development through a systematic approach to resilient, sustainable, and inclusive infrastructure.



The DRI Connect platform will be one of its kind in serving as the one-stop online space for DRI stakeholders to connect, learn and collaborate towards improved practices, processes and policies for resilient infrastructure systems. It will comprise of E-learning and Communities of Practice, Knowledge Portal and CDRI Resilient Infrastructure Marketplace

International Conference on Disaster Resilient Infrastructure (ICDRI) is the annual conference of CDRI bringing together experts, decision-makers and practitioners from Member Countries, organizations and institutions to discuss challenges and identify good practices to strengthen the global discourse on disaster and climate resilient infrastructure.















.jpg)


